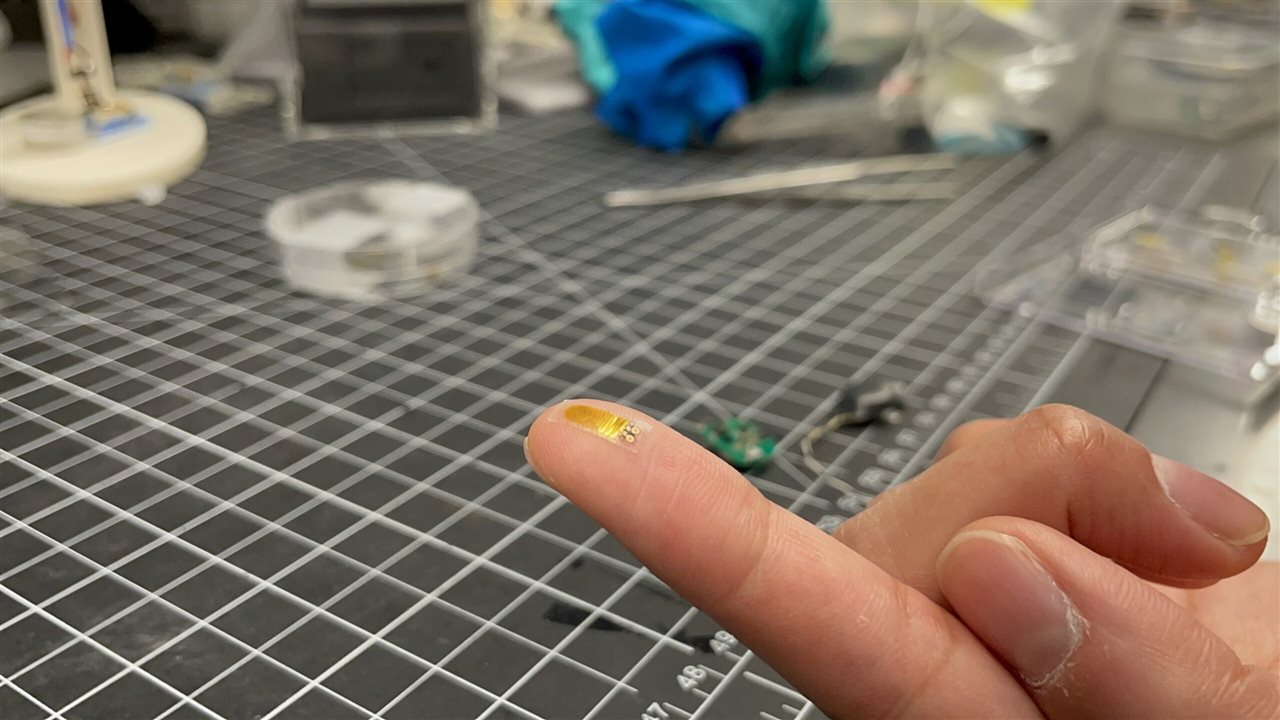
The ultra-tiny sensor can detect transplanted organ rejection up to three weeks earlier than traditional monitor techniques. (Image Credit: Northwestern University)
Northwestern University researchers developed a tiny soft device capable of monitoring transplanted organs for signs of rejection up to three weeks earlier than today's monitoring methods. They already implanted the sensor atop a model mouse's transplanted kidney, and it detected temperature irregularities related to inflammation and other bodily responses caused by transplant rejection. The device then notifies the physician or patient by wirelessly transmitting data to a smartphone or tablet. Physicians could find this beneficial because it allows them to respond quicker, improve patient outcomes/well-being, and preserve donated organs.
Once the organ is transplanted, rejection can occur anytime, even years later. It's a silent process, and patients may not have any symptoms. "If rejection is detected early, physicians can deliver anti-rejection therapies to improve the patient's health and prevent them from losing the donated organ," John A. Rogers, a bioelectronics pioneer who led the device development, said. "In worst-case scenarios, if rejection is ignored, it could be life-threatening. The earlier you can catch rejection and engage [in] therapies, the better. We developed this device with that in mind."

The entire electronic system. (Image Credit: Northwestern University)
Instead of measuring creatinine and blood urea nitrogen levels and taking biopsies to see how the kidney functions, physicians can use this new sensor, which takes a different approach. It measures temperature, which increases with inflammation. The team theorized that detecting unusual temperature variations and rising temperatures could be an early sign of transplant rejection.
The researchers verified this in their study with the mouse. In this case, the transplanted kidney's local temperature increased by up to 0.6° C at times, suggesting rejection is occurring. Animals that didn't consume immunosuppressant medications experienced temperature increases two or three days before biomarkers changed in blood samples. Meanwhile, those on immunosuppressant medications showed temperature increases and more variations three weeks before creatinine and blood urea nitrogen increased.
"Organ temperature fluctuates over a daily cycle under normal circumstances," Madhvapathy said. "We observed abnormal higher frequency temperature variations occurring over periods of 8 and 12 hours in cases of transplant rejection."
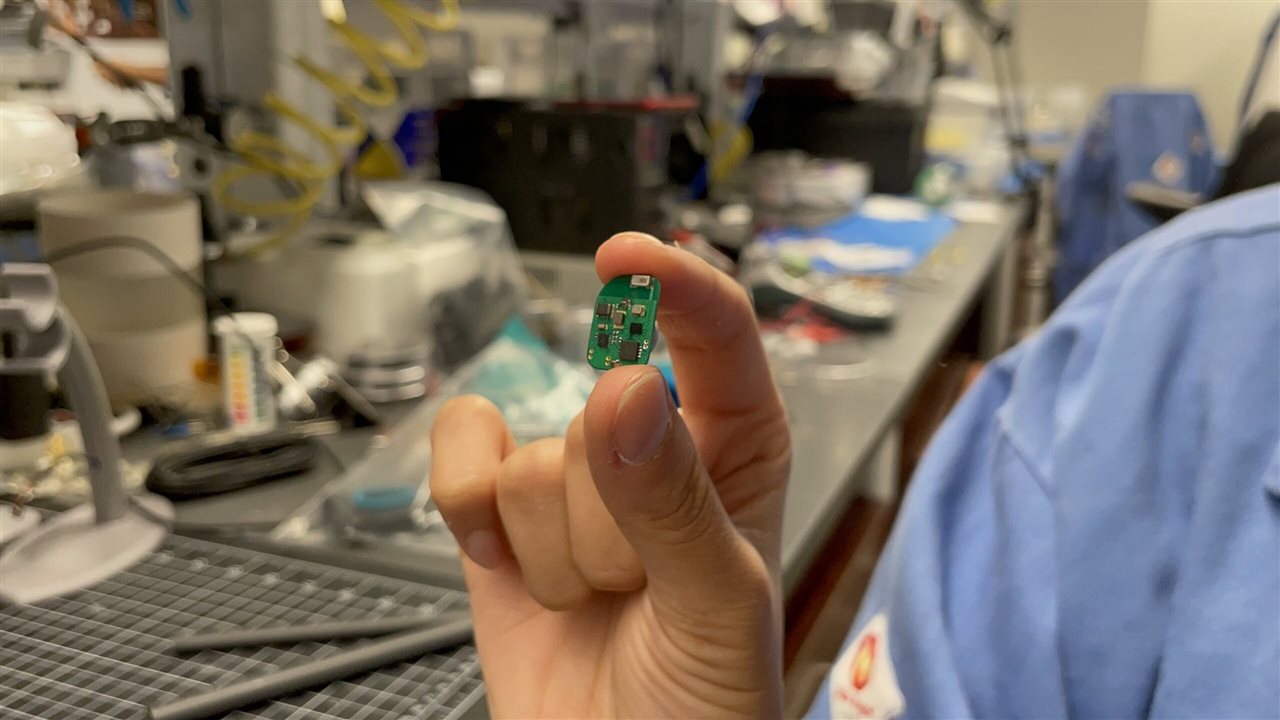
The system features a coin cell battery with Bluetooth to transmit data to a nearby device. (Image Credit: Northwestern University)
The team designed the tiny sensor (220 microns thick) to fit underneath the kidney's renal capsule layer, protecting the organ against damage. "The capsule keeps the device in good thermal contact with the underlying kidney," Rogers said. "Bodies move, so there is a lot of motion to deal with. Even the kidney itself moves. And it's soft tissue without good anchor points for sutures. These were daunting engineering challenges, but this device is a gentle, seamless interface that avoids risking damage to the organ."
The sensor features an ultra-sensitive thermometer that detects very slight kidney temperature variations (0.004 °C) and measures blood flow. However, the researchers concluded that temperature is a better indicator of rejection. Afterward, the sensors connect to electronics like a small coin cell battery for power that rests beside the kidney. It also uses Bluetooth to stream and send data to other devices.
"All electronic components are encased in a soft, biocompatible plastic that is gentle and flexible against the kidney's delicate tissues," Madhvapathy said. "The surgical insertion of the entire system, which is smaller than a quarter, is a quick and easy procedure."
Now, the team is testing the device on a bigger animal model. They're also exploring how the coin cell battery can recharge so the system runs throughout the patient's life. The team thinks this device could also work for other organs like the liver and lungs.
Have a story tip? Message me at: http://twitter.com/Cabe_Atwell
